Inside Efforts at VA, DOD for Enhanced Data Sharing in Health Care
Work across agencies are improving new tech and eyeing joint health information exchanges that make data more interoperable and transparent.
As the need to share data both within and outside of agencies grows, interoperability becomes critical to efficiently collaborate on key large-scale projects such as electronic health records and also delivering ideal patient care at the departments of Veterans Affairs and Defense.
About 97% of hospitals and 90% of physician offices across the country use electronic health records — a movement seen also within the federal government as it works to ensure agencies have the policies and capabilities to effectively share data to benefit patients.
“Interoperable health information technology improves patient care, enables better connection between patients and providers, helps reduce the risk of dangerous medical errors and makes sure that our country is prepared for any future public health care crisis,” Department of Health and Human Services’ Secretary Xavier Becerra said earlier this year regarding the importance of interoperable health networks.
Data Improves Mental Health Care
VA uses data and data analytics extensively in its mental health programs for clinical decision support, targeting treatments and to make care most accessible and effective for veterans.
The agency leverages its own and the Defense Department’s corporate data warehouses, which pull data from medical record instances and improve the clinical workflow. From this effort, VA has built data-driven prevention programs that use predictive analytics to estimate the risk of suicide in patients.
VA has launched two key suicide-prevention programs leveraging data: REACH VET and the Stratification Tool for Opioid Risk Management (STORM). Both programs have been very successful in reducing mortality in patients targeted by the programs’ treatment, according to Jodie Trafton, director of VA’s Program Evaluation and Resource Center within the Office of Mental Health and Suicide Prevention.
“[We] use predictive analytics to identify patients who look like patients who have died of suicide or had overdose or suicide events. We use that to estimate risk for our patient population and then create clinical tools that allow clinicians to go in, do case reviews on the patients we think look at high risk, and then do outreach or work with their treatment teams to try to optimize care delivery,” Trafton told GovCIO Media & Research in an interview. “They’re really helpful programs, combining predictive modeling with clinical care delivery to get better patient outcomes.”
VA has developed population management tools to better track high-risk patients and proactively monitor them, like the agency’s Suicide Prevention Population Risk Identification and Tracking for Exigencies (SPRITE) report. SPRITE tracks care engagement and risk mitigation interventions across a variety of patient populations at high risk of suicide, and links directly to a variety of additional decision support tools that support care protocols designed for specific conditions or care transitions.
VA also created a new dashboard to help with patient transitions from inpatient care to outpatient care, which improved successful transitions by 5%.
“SPRITE help us find if they’ve dropped out of services, haven’t been in touch with the VA for a while, find if they’ve stopped refilling their medications, if they’ve shown up in other facilities with emergency events, things like that. That allows our clinicians to keep tabs on all of the patients that they’re monitoring and make sure that they’re getting those treatments proactively,” Trafton said.
VA also collaborates with the Department of Energy to characterize risk and protective factors in social determinants of health and communities, then intertwines that information with VA’s data on patients and medical conditions.
“We find ways of partnering with communities to help improve care for veterans as well. So, we have a bunch of work now trying to integrate that medical record and outside data,” Trafton said.
The agency is integrating emerging technologies like natural language processing and high-performance computing to improve medical record search features as more information becomes digital.
“With these platforms, things that used to be hard to curate at volume — because we have about 1.7 million clinical notes coming per day — without those high-performance computing capacity, we weren’t able to do some of the things we’ve been able to implement now. So we’re pretty excited about that and what it means for being able to do more fancy, integrated analytics clinical care models,” Trafton said.
The Role of Joint Health Information Exchanges
The joint health information exchange implemented in April 2020 securely connects health and benefit information systems from the DOD, VA and other federal and private sector partners.
“It essentially expanded capabilities for both agencies to be able to improve patient safety and care coordination,” Cindy Pan from the Veterans Health Information Exchange Program Office and VA Exchange Partner Management Program Manager, told GovCIO Media & Research in an interview. “It serves as a common gateway for with participating external provider organizations.”
Organizations connected to the common gateway receive a single, aggregated health summary consisting of the patient’s VA and DOD health records, instead of having to send out multiple queries to get history from both agencies individually. In addition to the health summary, organizations can request more detailed health information like encounter summaries and clinical notes from the VA.
As of April 30, the joint health information exchange enabled real-time electronic health information sharing with about 274 external hospital systems. This includes approximately 2,600 hospitals, 40,000 clinics, 1,400 labs, 900 pharmacies, 1,000 federally qualified health centers and 34,000 provider sites.
“It packs a big punch,” Pan said. “We’re regularly bringing on new partners, and the networks that we’re connected to are constantly adding more participants. So our interoperability reach is really expanding on a regular basis. These real-time exchanges can lead to better patient care by reducing the need to carry paper medical records, which is something we can hopefully eliminate altogether.”
The improved transparency of a patient’s health record through the joint exchange enables a holistic view of a veteran’s medical history and is bolstered by VA’s Joint Longitudinal Viewer (JLV).
“Most of our VA staff use JLV to view the joint health information exchange records. So we have a widget within the JLV application that they use to see all those rich and robust records that are coming from the joint health information exchange. The same is true on the DOD side. It’s our window,” Rachel Wiebe, management and program analyst within VA’s JLV Office of Health Informatics/Health Solutions Management, told GovCIO Media & Research.
In April, VA had 1.2 million community documents opened in JLV, and VA is averaging between nine and 10,000 users per hour. VA also found that 47% of providers that use the system reported JLV always, most of the time, or usually prevents ordering of repeat diagnostics or medications.
“Not only do we know just intuitively that having access to complete records helps us coordinate care better, helps us have that holistic awareness of a patient’s entire longitudinal care situation, but we do have objective data that tells us that we’re doing something different because we have that information. We’re not duplicating tests and medications,” Wiebe added.
Since JLV’s inception 10 years ago, VA has continuously added more types of data the system shares. JLV includes records from the joint exchange, VistA CPRS, VistA imaging, Oracle Cerner, the newly added MUSE cardiology studies, the DOD’s legacy EHR systems and the Individual Longitudinal Exposure Record (ILER).
“JLV is using FHIR APIs. All of the data for both the VA and DOD Cerner implementations are stored in the same Millennium instance, so querying that, and bringing back all the records from the MHS Genesis implementation at DOD and the VA EHRM implementation at VA,” Wiebe said. “[With ILER], we’re now able to have a complete summary of the service members exposures while they were in active duty.”
Especially after the passage of the PACT Act last August, the Veterans Benefits Administration is leveraging JLV to provide evidence for claims and improve claims processing. Also, within the past year, JLV is bringing in the DOD Enterprise Central Image Archive.
“The power here is you’re not going to look for what’s coming from DOD, what’s coming from Cerner, what’s coming from VistA. … All of the systems are presented for you here and in single, integrated view,” Wiebe said. “Users can select domains or widgets they want on their workspaces. They can customize their workspaces. … We also like to emphasize the transparency of JLV it calls out for data, which it does real time, if JLV can’t reach something, it indicates a yellow triangle to the user and tells them what data they couldn’t access.”
Next Steps for Data Sharing at the Agencies
Moving forward, VA is continuing to advance their data sharing initiatives to “meet patients where they are,” Pan said.
As of today, VA is currently connected to eHealth Exchange and CommonWell Health Alliance. The agency is actively working with DOD on participation in the Carequality Interoperability framework and is targeting adoption of Office of the National Coordinator for Health IT (ONC)’s Trusted Exchange Framework and Common Agreement (TEFCA) published in 2022.
TEFCA aims to establish a universal technical and legal baseline for information exchange and interoperability across qualified health information networks (QHINs) nationwide.
“With TEFCA, ONC is essentially harnessing all that [interoperability] progress and putting into a national framework that we can all exchange through, and establish more standards through, so that everyone follows the same rules of the road. That always makes things smoother,” Pan said. “We’re definitely staying at the forefront of the edge trying to figure out how it’s going to affect us and our entire industry.”
In addition to TEFCA, VA is driving a handful of internal priorities like optimization with the joint exchange, and collaborating with VA’s JLV team and DOD partners to shorten return documents and improve how documents are read.
“We’re constantly taking feedback and working with all of the stakeholders to improve the system,” Pan said. “We also want to implement additional exchange purposes. … For example, our current exchange agreement in place between the VA and the Social Security Administration (SSA) has reduced the claims processing time for SSA disability benefit claims from multiple weeks just a matter of days. We’d really like to see that level of efficiency and apply it to other areas. So expanding and utilizing the system that we’ve already built to be able to benefit other purposes of use at other agencies.”
This is a carousel with manually rotating slides. Use Next and Previous buttons to navigate or jump to a slide with the slide dots
-
Federal Agencies Make the Case for Quantum
Amid development of emerging technologies like AI and machine learning, leaders see promise in quantum computing.
6m read -

NCI Program Unlocks Emerging Proteomic Data to Advance Precision Medicine
Researchers say sharing molecular cancer research data can expand cancer treatment and care.
32m listen -

Cyber Resilience and Recovery Amid Evolving Cyber Threats
Data durability is a key aspect of NIST’s cybersecurity framework for public and private organizations.
21m listen -
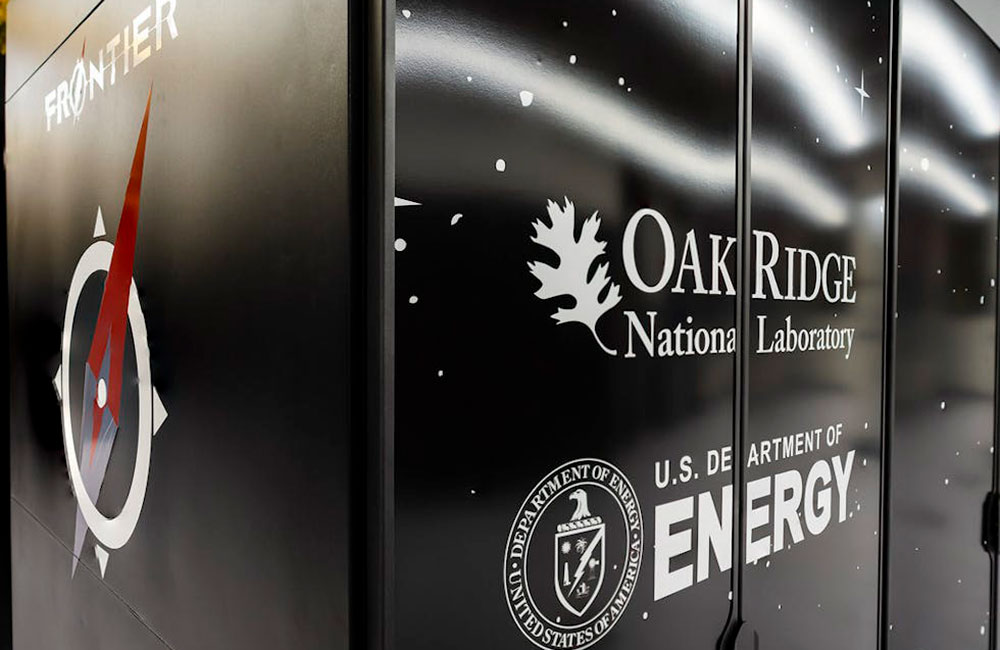
Energy Researchers Aim For Holistic Approach to AI Issues
A new center at the Oak Ridge National Laboratory is looking at under-researched areas of AI to better understand how to secure it.
2m read




